SELECTIVE SPINAL CORD LESIONING PROCEDURES FOR PAIN
In the 1960s, a large number of neurophysiologic investigations proved
that the dorsal horn was the primary level of modulation of pain
sensation. This idea was popularized in 1965 through the gate control
theory, which drew neurosurgeons’ attention to this area as a possible
target for pain surgery. Neurostimulation of the primary afferent
neurons was developed to enhance the inhibitory mechanisms of the spinal
cord. Conversely, in 1972 anatomical studies were undertaken and
preliminary surgical trials in the human dorsal root entry zone (DREZ)
to determine whether a destructive procedure at this level was feasible.
Soon after, in 1974, Nashold and his group started to develop DREZ
lesions using the RF thermocoagulation as the lesion maker in the
substantia gelatinosa of the dorsal horn and later in the whole DREZ.
This has been performed especially for pain caused by brachial plexus
avulsion. Later on, DREZ procedures were performed by using a laser and
an ultrasound probe for pain caused by brachial plexus avulsion.
 MICROSURGICAL DREZotomy
MICROSURGICAL DREZotomy
This procedure consists of a longitudinal incision of the dorsolateral
sulcus ventrolaterally at the entrance of the rootlets into the sulcus.
Microbipolar coagulations are performed continuously inside the sulcus
down to the apex of the dorsal horn and along all the spinal cord
segments selected for surgery. The lesion, which penetrates the lateral
part of the DREZ and the medial part of the tract of Lissauer (TL),
extends down to the apex of the dorsal horn, which can be recognized by
its brown-gray color. The average lesion is 2 to 3 mm deep and is made
at a 35° angle medially and ventrally.
The procedure is presumed to preferentially destroy the nociceptive
fibers grouped in the lateral bundle of the dorsal rootlets, as well as
the excitatory medial part of the TL. The upper layers of the dorsal
horn are also destroyed if microbipolar coagulations are made inside the
dorsal horn . The upper layers of the dorsal horn are known to be the
site of “hyperactive” neurons, especially in the cases with peripheral
deafferentation (Fig.1). The procedure is presumed to at least partially
preserve the inhibitory structures of the DREZ, (i.e., the lemniscal
fibers reaching the dorsal column, as well as their recurrent
collaterals to the dorsal horn and the substantia gelatinosa [SG]
propriospinal interconnecting fibers running through the lateral part of
the TL). This MDT was
conceived in order to prevent the complete abolition of tactile and
proprioceptive
sensations and to avoid deafferentation phenomena.
| |
 |
|
| |
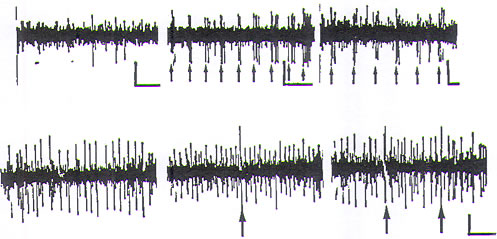
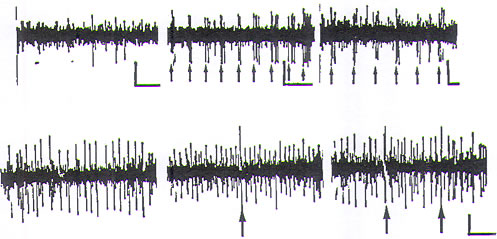
FIGURE.1 Dorsal horn microelectrode recordings in man. The electrode
was a floating tungsten
microelectrode that was implanted intraoperatively free-hand under the
operative microscope;
it reached 5 mm in depth (in laminae IV–VI). The vertical bars are 50 μV,
and the horizontal bars
are 100 ms. Upper trace, normal activity. Recordings in a
nondeafferented dorsal horn (spastic
patient). Left, almost no spontaneous activity (3 spikes at random).
Middle, spike burst discharges
(arrows) evoked by regular light tactile stimulation of the
corresponding dermatoma. Right, electrical
stimulation of the corresponding peripheral nerve. Lower trace,
deafferentation hyperactivity.
Recordings in the L5 cord segment of a patient with pain caused by a
traumatic section of the
hemi-cauda equina from root L4 to S4. Left, spontaneous activity of the
recorded unit: continuous,
regular, high-frequency discharge. Middle, unit during light tactile
stimulation of the L4–S1 dermatome
(arrow). Right, during electrical stimulation of the tibial nerve (the
arrows are two consecutive
stimuli). Note the continuous regular discharges, which remain
unaltered. |
|
Working in the DREZ requires knowledge of the morphological anatomy of
the dorsal roots corresponding to the spinal level. The axis of the dorsal horn in
relation to
the sagittal plan crossing the dorsolateral sulcus will condition the
angulation
of the DREZotomy. According to 82 measurements performed by Young, the mean DREZ angle is 30° at C6, 26° at
T4, 37° at T12, and 36° at L3. The site and extent of the DREZ lesion
will
also be determined by the shape, width, and depth of the TL and dorsal
horn
(Fig.2).
 Surgery is performed with the patient under general anesthesia, but with
only an initial short-lasting muscle relaxant to allow intraoperative
observation
of motor responses to bipolar electrical stimulation of the nerve roots.
Stimulated ventral roots have a motor threshold at least three times
lower than
the dorsal roots. Standard microsurgical techniques are used with 10× to
25×
magnification.
Surgery is performed with the patient under general anesthesia, but with
only an initial short-lasting muscle relaxant to allow intraoperative
observation
of motor responses to bipolar electrical stimulation of the nerve roots.
Stimulated ventral roots have a motor threshold at least three times
lower than
the dorsal roots. Standard microsurgical techniques are used with 10× to
25×
magnification.
 OPERATIVE PROCEDURE AT THE CERVICAL LEVEL
OPERATIVE PROCEDURE AT THE CERVICAL LEVEL
The prone position with the head and neck flexed in the “concorde”
position
has the advantage of avoiding brain collapse caused by cerebral spinal
fluid
(CSF) depletion. The head is fixed with a three-pin head holder. The
level of
laminectomy is determined after identification of the prominent spinous
process of C2 by palpation. A hemilaminectomy, generally from C4 to C7,
with
preservation of the spinous processes, allows sufficient exposure to the
posterolateral
aspect of the cervical spinal cord segments that correspond to the
upper limb innervation, that is, the rootlets of C5 to T1 (T2).
After the dura and the arachnoid are opened longitudinally, the exposed
roots and rootlets are dissected free by separation of the tiny
arachnoid filaments
that bind them to each other, to the arachnoid sheath, and to the spinal
cord pia mater. The radicular vessels are preserved.
Each ventral and dorsal root from C4 to T1 is electrically stimulated at
the
level of its corresponding foramen to precisely identify its muscular
innervation
and its functional value. Responses are in the diaphragm for C4 (the
response
is palpable below the lower ribs), in the shoulder abductors for C5, in
the elbow
flexors for C6, in the elbow and wrist extensors for C7, and in the
muscles of
the hand for C8 and T1.
Microsurgical lesions are performed at selected levels that correspond
to the pain territory. The incision is made with a microknife. Then
microcoagulations
are made in a “chain” (i.e., dotted) manner. Each microcoagulation is
performed
by short-duration (a few seconds), low-intensity, bipolar
electrocoagulation
with a special sharp bipolar forceps. The depth and extent of the lesion
depend on the degree of the desired therapeutic effect and the
preoperative sensory
status of the patient.
| |
 |
|
| |
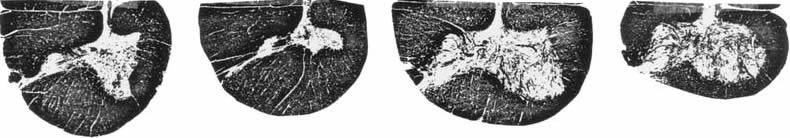
FIGURE.2 Variations of shape, width, and depth of the DREZ area,
according to the spinal cord
level (from left to right: cervical n° 7, thoracic n° 5, lumbar n° 4,
sacral n° 3). Note how, at the
thoracic level, Lissauer’s tract is narrow and the dorsal horn deep.
Therefore, it is easy to understand
that DREZ lesions at this level can be dangerous for the corticospinal
tract and the dorsal
column. |
|
If the laxity of the root is sufficient, the sulcotomy is accomplished
through
an incision performed continuously in the dorsolateral sulcus,
ventrolaterally
along all of the rootlets of the targeted root. If this is not the case,
a partial ventrolateral
section is made successively on each rootlet of the root after the
surgeon
has isolated each one by separation of the tiny arachnoid membranes that
hold them together.
For pain due to brachial plexus avulsion, dotted microcoagulations
inside
the dorsal horn (at least 3 mm in depth from the surface of the cord)
are performed
after incision of the dorsolateral sulcus. Sharp graduated bipolar
forceps
are used to make the microcoagulations at the level of the avulsed
roots. Selective
ventrolateral DREZ lesions are extended to the root remaining above and
below. In brachial plexus avulsion, dissection of the spinal cord is
sometimes
difficult to achieve safely because of scar tissue adhering to the cord.
Atrophy
and/or gliotic changes at the level of the avulsed roots can make
identification
of the dorsolateral sulcus hazardous. In such cases, it is necessary to
start from
the roots remaining above and below. The presence of tiny radicular
vessels that
enter the cord may help determine the site of the sulcus. Yellow areas
corresponding
to old hemorrhages on the surface of the cord and/or microcavities in
the depth of the sulcus and the dorsal horn provide some guidance for
tracing
the sulcomyelotomy. When the dorsolateral sulcus is difficult to find, intraoperative
monitoring of the dorsal column somatosensory evoked potentials
(SEPs) evoked by stimulation of the tibial nerve is especially helpful.
 OPERATIVE PROCEDURE AT THE
LUMBOSACRAL LEVEL
OPERATIVE PROCEDURE AT THE
LUMBOSACRAL LEVEL
The patient is positioned prone on thoracic and iliac supports, and the
head is
placed 20 cm lower than the level of the surgical wound to minimize the
intraoperative
loss of CSF. The desired vertebral level is identified by palpation of
the spinous processes or, if this is difficult, by a lateral x-ray study
that includes
the S1 vertebra. Interspinous levels identified by a needle can then be
marked
with methylene blue. A laminectomy—either bilateral or unilateral,
according
to pain topography—from T11 to L1 (or L2) is performed. The dura and
arachnoid
are opened longitudinally and the filum terminale is isolated. Roots are
then identified by electrical stimulation.
The L1 and L2 roots are easily identified at their penetration into
their
respective dural sheaths. Stimulation of L2 produces a response of the
iliopsoas
and adductor muscles.
Identification of L3 to L5 is difficult for many reasons: (1) the exit
through
their respective dural sheaths is caudal to the exposure; (2) the dorsal
rootlets
enter the DREZ along an uninterrupted line; (3) the ventral roots are
hidden in
front of the dentate ligament; and (4) the motor responses in the leg to
stimulation
of the roots are difficult to observe intraoperatively because of the
patient’s
prone position. Stimulation of L3 produces a preferential response in
the adductors
and quadriceps, of L4 in quadriceps, and of L5 in the tibialis anterior
muscle.
Stimulation of the S1 dorsal root produces a motor response of the
gastrocnemius-
soleus group that can be confirmed later by repeatedly checking the
Achilles ankle reflex before, during, and after MDT at this level.
Stimulation of the S2–S4 dorsal roots (or better, the corresponding
spinal
cord segments directly) can be assessed by recording the motor vesical
or anal
response by use of cystomanometry, rectomanometry, or electromyography
of
the anal sphincter (or by inserting a finger into the rectum). Because
neurophysiological
investigations are time-consuming to perform in the operating
room, measurements at the conus medullaris can be
sufficient
in patients who already have severe preoperative impairment of their
vesicoanal
functions. These measurements, based on human postmortem
anatomical studies, have shown that the landmark between the S1 and S2
segments
is situated around 30 mm above the exit from the conus of the tiny
coccygeal
root.
At the lumbosacral level, MDT is difficult and possibly dangerous
because of
the rich vasculature of the conus. The posterolateral spinal artery
courses along
the posterolateral sulcus. Its diameter is between 0.1 and 0.5 mm, and
it is fed
by the posterior radicular arteries. It joins caudally with the
descending anterior
branch of the Adamkiewicz artery through the conus medullaris
anastomotic
loop of Lazorthes. If it is freed from the sulcus, this artery can be
preserved.
 NEUROPHYSIOLOGICAL MONITORING AS AN AID TO SURGERY
NEUROPHYSIOLOGICAL MONITORING AS AN AID TO SURGERY
Intraoperative monitoring of SEPs can be performed at the surface of the
exposed spinal cord. Recordings of presynaptic potentials from the
dorsal root
and postsynaptic potentials from the dorsal horn can be useful for
identification
of the spinal cord segments. Potentials have a maximal amplitude in
C6–C7
stimulation of the median nerve and the C8 segment for stimulation of
the
ulnar nerve. They have a maximum amplitude in the L5–S2 segments for
stimulation
of the tibial nerve, and in the S2–S4 segments for stimulation of the
dorsal nerve of the penis or clitoris.
| |
 |
|
| |
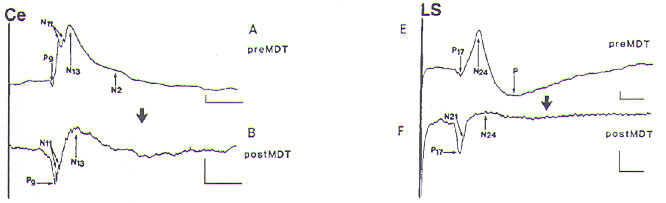
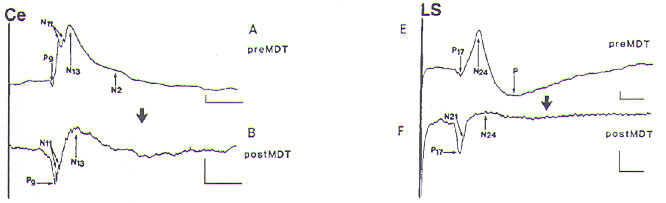
FIGURE.3 Effects of MDT on the evoked electrospinogram (EESG).
Recordings from the surface
of the dorsal column, medially to the DREZ at the C7 cervical (Ce) and
the L5 lumbosacral
(LS) segments, ipsilateral to the stimulation of the median and the
tibial nerve, respectively, before
(A) and after (B) MDT. The initial positive event P9 (for cervical) (P17
for lumbosacral) corresponds
to the far-field compound potential originating in the proximal part of
the brachial (lumbosacral)
plexus. The small and sharp negative peaks N11 (N21) correspond to
near-field presynaptic
successive axonal events, probably generated in the proximal portion of
the dorsal root, the dorsal
funiculus, and the large-diameter afferent collaterals to the dorsal
horn. After MDT, all of these
presynaptic potentials remain unchanged. The larger slow negative wave
N13 (N24) corresponds
to the postsynaptic activation of the dorsal horn by group I and II
peripheral afferent fibers of the
median (tibial) nerves. They are diminished after MDT (in the order of
two thirds). The later negative
slow wave N2 (just visible in the cervical recording) corresponds to
postsynaptic dorsal horn
activity consecutive to the activation of group II and III afferent
fibers. N2 is suppressed after MDT. |
|
Recordings of surface spinal cord SEPs can also be helpful in monitoring
the
surgical lesion itself. Dorsal column potentials can be monitored to
check the
integrity of the ascending dorsal column fibers, especially when the
dorsolateral
sulcus is not clearly marked (as is common in brachial root avulsion).
The dorsal
horn potentials can be monitored to follow the extent of MDT,
particularly when
good sensory functions are present before surgery.
 MICROELECTROPHYSIOLOGY
AND MICRODIALYSIS STUDIES IN THE DORSAL
HORN DURING SURGERY
MICROELECTROPHYSIOLOGY
AND MICRODIALYSIS STUDIES IN THE DORSAL
HORN DURING SURGERY
Unitary spikes generated in the dorsal horn neurons are interesting to
record
during DREZotomy to indicate abnormal activities, to help identify the
surgical
target, and to better understand the electrophysiological mechanisms
underlying
painful phenomena. Toward this goal, one group has developed
special, simplified floating microelectrodes. At the beginning, these
electrodes
were based on the design by Merril and Ainsworth, and later they
were
developed into an original design (i.e., a double microelectrode with an
enhanced ability to distinguish spikes from artifacts). In this way,
they
conducted recordings in 25 patients. To learn about specific patterns
recorded
from deafferented neurons, more patients must be studied. The group has performed
microdialysis studies in the dorsal horn of patients undergoing
DREZotomy. The aim of the work was to measure concentrations of some of the
main
neurotransmitters hypothesized from the animal experiments to be present
in
the human dorsal horn. The microprobe has an apical 4-mm-long tubular
membrane [diameter: 0.216 mm, Cuprophane (HOSPAL Industrie, Meyzieu,
France), cutoff 6000 Da]. The probe is perfused at 2 μl/min with a
Ringer solution.
Dialysate fractions are collected from the extracellular fluid every 5
min
for about 1 hr. All the samples are frozen for later analysis [high
performance
liquid chromatography (HPLC) with fluometric detection]. At the present
time they have made the technique feasible for identification and dosages of
the following
substances: glutamate, aspartate, GABA, glycine, taurine, serine, and
threonine.
The preliminary results indicate some differences between painful and
nonpainful
states. Further studies are needed before giving conclusions.
 RADIOFREQUENCY (RF)
THERMOCOAGULATION PROCEDURE
RADIOFREQUENCY (RF)
THERMOCOAGULATION PROCEDURE
In 1976 Nashold and his group published data on a method using RF
thermocoagulation to destroy hyperactive neurons in the substantia
gelatinosa
and in 1979 in the whole DREZ region. In 1981 the technique
was
modified to produce less extensive lesioning so that the risk of
encroachment
into the neighboring corticospinal tract and dorsal column would be
minimized.
With the modified technique, the lesion is made with a 0.5 mm insulated
stainless steel electrode with a tapered noninsulated 2 mm tip, designed
and manufactured by Radionics Inc. (Burlington, MA).
For treatment of pain after brachial plexus avulsion, the electrode
penetrates
the dorsolateral sulcus to a depth of 2 mm at an angle of 25–45° in the
lateral–
medial direction. A series of RF coagulations are made under a current
of
35–40 mA (not over 75°C) for 10–15 s. The RF lesions are spaced at 2–3
mm
intervals along the longitudinal extent of the dorsolateral sulcus. The
lesion
observed under magnification is seen as a circular whitened area that
extends
1–2 mm beyond the tip of the electrode.
In a recent publication, Nashold emphasizes the importance of obtaining
impedance measurements from tissue during surgery. Before and after
each lesion is made, the impedance has to be measured. It is usually
less
than 1200 Ω in a damaged spinal cord. The authors state that as the
transition
from injured parenchyma into more normal tissue is made, impedance
readings should increase and eventually reach normal levels of 1500 Ω.
The
authors use these numbers as a guide to stop the lesion making at the
desired
end.
 DREZ PROCEDURES WITH THE LASER BEAM
DREZ PROCEDURES WITH THE LASER BEAM
Levy et al. in 1983 and Powers et al. in 1984 advocated CO2
and
argon lasers, respectively, as lesion makers. According to Levy et al.’s
description,
the pulse duration of the CO2 laser is 0.1 sec and the power is adjusted
to about 20 W, so that one or two single pulses create a 2 mm depression
at
a 45° angle in the DREZ. The lesions are probed with a microinstrument
marked at 1 mm increments to ensure that the depth of the lesions (1–2
mm)
is adequate.
Intraoperative observations in humans and experimental studies comparing
DREZ lesions performed with the RF thermocoagulation to those made with
various laser beams found that the laser lesions were generally
more circumscribed
and less variable. Walker et al., on the other hand, reported
on the danger of creating extensive damage and syrinx cavities with the
laser
(CO2). In a well-documented study evaluating the effects of DREZ lesions
with
RF or CO2 on the dog spinal cord, Young found that the size and
extent
of the lesion related primarily to the magnitude of power used to make
the
lesion. They showed that by using any of the three techniques, the
lesions
could be successfully localized to the DREZ (including the layers I–VI
of the
dorsal horn) and the dorsal column and the corticospinal tract spared.
The main
difference was that with the laser, the lesion was shaped like the
letter “V”, with
the maximum width at the surface, whereas with RF it tended to be more
spherical.The same glial reactions were observed using both methods in chronic
animal models.
Young, in his series of patients, made a comparative analysis of RF
and
CO2-laser procedures. With RF, 39 of the 58 patients (67%) reported good
results (pain regressed by 50% or more) and with the CO2 laser, 9 out of
the 20
patients (45%) reported good results. Postoperative complications with
RF
were noted in 26%, and with CO2 laser in 15%.
 ULTRASONIC DREZ PROCEDURE
ULTRASONIC DREZ PROCEDURE
This procedure was developed by Kandel and Dreval in Moscow. It
has been mostly used for pain caused by brachial plexus avulsion.
According
to the description given by Dreval, the technique consists of a
continuous longitudinal
opening of the dorsolateral sulcus at the level of the avulsed roots
to the depth of the microcavities and the changed spongy cord tissue. At
the
same time, ultrasonic destruction of the pathological tissues is done.
The
lesion is strictly in the projection of the dorsolateral sulcus at an
angle of 25°
medially and ventrally. The depth of the microcavities is the main
criterion
of the depth of the lesioning. After ultrasonic DREZ sulcomyelotomy, the
grey color of the dorsal horn is well seen in the depth of the opened
dorsolateral
sulcus. The vessels crossing the sulcus are kept intact. The ultrasonic
lesions are produced at a working frequency of 44 kHz, and the amplitude
of
ultrasonic oscillation is 15–50 μm. The lesions are placed in a “chain”
manner
along the sulcus.
 INDICATIONS FOR DREZ
INDICATIONS FOR DREZ
Indications are as follows:
1. Cancer pain that is limited in extent (such as in Pancoast-Tobias
syndrome).
2. Persistent neurogenic pain that is due to:
A) Brachial plexus injuries, especially those with avulsion.
B) Spinal cord lesions, especially for pain corresponding to segmental
lesions. Pain below the lesion is not favorably influenced. Segmental
pain caused by lesions in the conus medullaris and the cauda equina
is significantly relieved. Pain due to cauda equina lesions can also
be indications.
C) Peripheral nerve injuries, amputation, and herpes zoster, when the
predominant component of pain is of the paroxysmal type and/or
corresponds to provoked allodynia hyperalgesia.
3. Disabling hyperspasticity with pain.
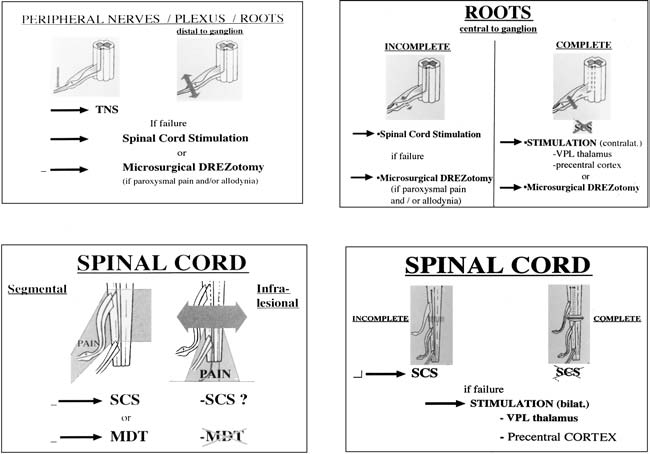
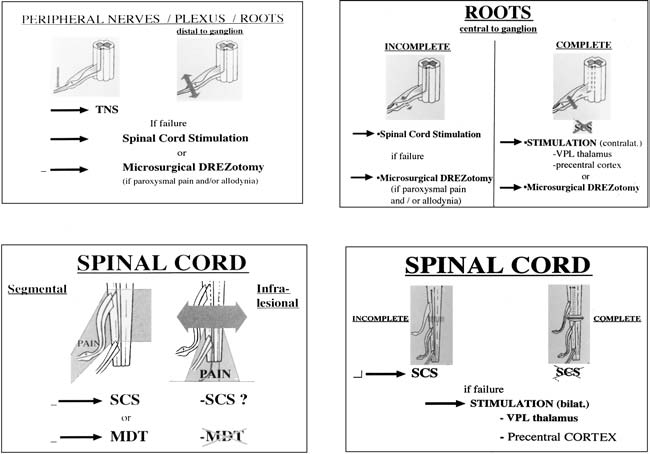
Surgery in the DREZ must be considered alongside other methods belonging
to the armamentarium of pain surgery. Figure.4 summarizes present
process of decision making for neuropathic pain.
| |
 |
|
| |
FIGURE.4 Decision making for
neuropathic pain, originating from the following:
upper left, peripheral nerves, plexus, roots distal
to ganglion lesions; upper right, roots central to
ganglion lesions; lower right, incomplete and
complete spinal cord lesions; lower left, treatment
for the segmental and the infralesional components
of the pain are different. |
|
|


 Surgery is performed with the patient under general anesthesia, but with
only an initial short-lasting muscle relaxant to allow intraoperative
observation
of motor responses to bipolar electrical stimulation of the nerve roots.
Stimulated ventral roots have a motor threshold at least three times
lower than
the dorsal roots. Standard microsurgical techniques are used with 10× to
25×
magnification.
Surgery is performed with the patient under general anesthesia, but with
only an initial short-lasting muscle relaxant to allow intraoperative
observation
of motor responses to bipolar electrical stimulation of the nerve roots.
Stimulated ventral roots have a motor threshold at least three times
lower than
the dorsal roots. Standard microsurgical techniques are used with 10× to
25×
magnification.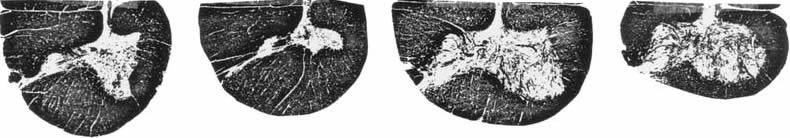
 What’s Up
What’s Up